The Role of 5G in Smartwatches Faster Connectivity and More

Screen Rant
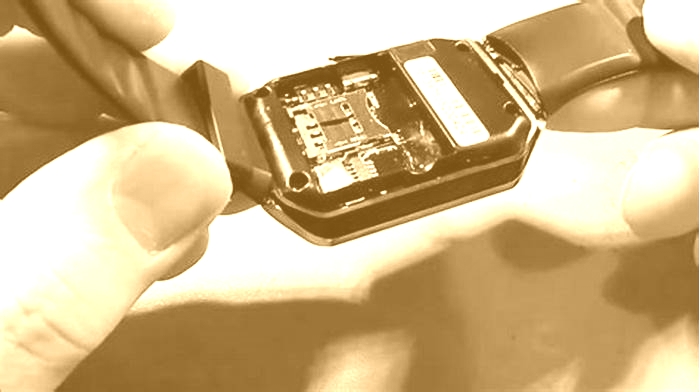
Qualcomm has announced a new chip that will deliver 5G capabilities to IoT devices, including smartwatches, but do people really need super-fast connectivity on their wrists? Over the past few years, 5G has become the preeminent cellular network globally, replacing LTE. It offers much faster connections than 4G, helping people accomplish more on their smartphones and tablets, even when they are not connected to Wi-Fi. Most smartphones launched today offer 5G connectivity, although most IoT devices still only support LTE networks.
According to Qualcomm, the Snapdragon X35 chip is the worlds first 5G NR-Light modem-RF system for IoT devices, XR glasses, and smartwatches that dont require the power and performance of 5G smartphones but can still benefit from the inherent advantages of 5G technology. This includes lower latency, increased battery life, and improved uplink speeds. NR-Light is a new 5G standard that aims to fill the gap between high-speed mobile broadband devices and extremely low-bandwidth NB-IoT devices. Qualcomm says that the Snapdragon X35 will be offered to OEMs by this summer, and consumer devices carrying the new chip will hit the market early next year.
Related: What Does 5G UW Mean On iPhone And Android?
Moving From LTE To 5G Connectivity
With LTE connectivity still not available with all smartwatches, the concept of 5G support on a wearable could seem a little too gratuitous for some, especially because people do not normally stream high-definition videos or play heavy-duty games on their smartwatches. However, contrary to popular perception, 5G offers much more than high speed. For starters, 5G has much lower latency than LTE, helping devices make quicker connections across the internet.
Another major benefit of 5G is the higher bandwidth that could help multiple devices connect to the internet simultaneously. It is especially helpful in the IoT scheme of things, with connected gadgets, appliances, and wearables becoming more common every year. The additional bandwidth can help many people stay connected to the cellular network in busy places like airports, theaters, stadiums, and more.
Another reason why 5G needs to be adopted more widely by IoT devices and wearables is that it is the future of cellular connectivity. 4G will eventually go the way of 2G and 3G networks someday, and modern gadgets will be much more future-proof if they ship with 5G support. Currently, 4G networks are already impeding 5G expansion efforts, since they share most of the common low-band frequencies with 5G networks. Once 4G networks are phased out, low-band frequencies will be fully available to 5G networks, helping the latter attain its true potential. So while a 5G-enabled smartwatch may not be a must-have right now, it will certainly be a step in the right direction.
More: What Does 5G UC Mean On Android?
Source: Qualcomm
5G Use in Healthcare: The Future is Present
1. Communication Basic Principles
5G technical Parameters
Currently, mobile data transmission is mainly based on 4G/LTE or on Wi-Fi. The 4G/Long-Term Evolution (LTE) offers a minimum signal delay of 20ms mainly designed for internet (e.g., browsing and video streaming) which is well below that required for real-time integration of sensor data. Furthermore, Wi-Fi solutions are an alternative, but they can be interrupted by other users at any time due to unprotected radio bands.11
The new 5G telecommunication standard offers high bandwidths as compared to the current mobile transmission standard 4G/LTE: 5G is a 100 times higher data transmission rate (up to 10GB/s), and, at the same time, an extremely low latency time (<1ms), and 1000 times higher capacity (bandwidth) with a high quality of service which is almost equal to the zero data response time in the real world.12 Millimeter wave telecommunication is such an advantageous technology for 5G networks because it allows extremely high data transfer speeds (several gigabits per second). However, a large number of small cells with limited radius deployment must be used to achieve seamless and efficient coverage and form a 5G ultradense cellular network. The cells may be of different size, and they are classified as Femtocells, Picocells or Microcells. The massive multi-input, multioutput is an evolving technology capable to transmit multiple data beams at a time, thus increasing the throughput and spectrum effectiveness in both uplink and downlink.13
Additionally, 5G requires up to 10 times less energy than the previous 4G/LTE mobile communications standard.12 It is expected that the 5G network will have a 1,000-fold rise in traffic in the coming decade, although the energy usage of the whole infrastructure will be just half of todays system's consumption. Therefore, this is a crucial factor for reducing the total cost of ownership, including the environmental impact of the networks.13
The above mentioned qualifications meet the requirements imposed by many new digital applications like the interconnection between physical and virtual objects, the IoT, autonomous driving,14 machine-to machine connection in industrial production,15 as well as different medical applications that were previously technically impossible to implement.16 The latter systems conform to the Ultrareliable low-latency communication protocol where a sub-millisecond latency with a response rate smaller than 1 packet loss in 105 packets is required for patient safety.17
To achieve their goals, the industry reached a consensus to use emerging major technologies like network function virtualization (NFV) and software-defined networking (SDN). The most remarkable technology to simplify a healthcare network management is SDN, which takes apart the network control from the data forwarding plane. Thus, the control plane oversees the entire network below as well as the network resources by using a programmable Application Programming Interface (API) .17
As 5G is expected to greatly influence our lives, its security is even more important than before. Two types of 5G network security are implemented:
Security using software such as firewall applications installed in the perimeter of any network, based on need.
AI-based security as it can sensibly identify the terminal actions and requirements on time to avoid service interruptions.
In order to further enhance the security one can also use security automation and Blockchain security assessment techniques.17
The 5G network requires more complex antenna design and distribution in the space needed to be covered in order to achieve faster speeds and low latency. Therefore, specific antennas are proposed for the 5G network, also known as active antennas (in contrast to passive antennas used in 4G) which differentiate 5G network in terms of speed, latency, and security.
Recently, big international telecommunication companies have taken the lead in the competition for the upcoming 5G cellular technology, as it is thought to be their most important future source of revenue. It is expected that the 5G network will be broadly introduced as a simple framework for hyperconnected mobile devices and will ultimately evolve into a modern 5G platform. It should be noted, however, that there is currently no uniform 5G standard. For a detailed technical review of the architecture and security of 5G Technology, the reader can refer to reference.17
Looking beyond 5G, the future generation of telecommunications (6G), is already in the late research and development (R&D) phases (Technology Readiness Levels - TRL 35), with an exponential increase in bandwidth and capabilities that will allow implementation of applications that even 5G cannot fulfil (). This is especially important in the area of network security/privacy and maintaining Healthcare Insurance Portability and Accountability Act (HIPAA)5 compliance.
Table 2.
Parameters of Current and Next Generations of Telecommunications*
| Generation | Bandwidth | Speed | Latency |
|---|---|---|---|
| Current 4G | 5200MHz | 1050 megabits per second | 5060ms |
| 20202030 5G | 1 23 GHz | 10200 gigabits per second | 110ms |
| 20302040 6G | 17 THz | 17 terabits per second | 110 ms |
With the current full life cycle development of a technology product from concept to commercialization at 1015years, it is likely that the 6G may be available within that time period, or perhaps slightly sooner. With integration of other advanced technologies, such as smart devices, composed of micro-electro-mechanical-systems (MEMS) sensors, AI and computational analytics on a single chip, automatic diagnosis can be immediately generated at the point of care (edge computing) and transmitted to a waiting consulting physician or directly to the electronic medical record. Another emerging area of 6G, will support virtual reality (VR), where a simulated presence is generated by computer graphics and allows users to interact with the simulated elements in a seemingly real way. Augmented reality (AR), where computer-aided information is generated and graphically augmented (overlayed) to the display real-time, can also have broad implications for healthcare. Counselling patients and preoperative consent can likely be enhanced with augmented reality, and nonclinical functions in hospitals such as navigation, in particular for visually impaired patients.5 Both humans and machines will use 6G which will allow for truly immersive extended reality (XR) and high-fidelity mobile hologram which could have enormous implications for healthcare; but although the 6G networking will provide ample potential for VR/AR or even XR, the immersive experience of these alternative realities has yet to find a practical application within the clinical healthcare field.
Telemedicine
The most use of 5G networks in healthcare is currently Telemedicine, and when the world emerges from global COVID-19 pandemic, healthcare will become a hybrid medical practice of live face-to-face clinical care and telemedicine-based care.
The World Health Organization (WHO) has announced COVID-19 was a pandemic (World Health Organization,2020). With the nonlinear rapid disease expansion, COVID-19 has caused widespread healthcare, socio-political and economic impact.1820 Countries and healthcare systems around the world have been forced to rapidly adapt to telehealth and digital innovations to mitigate the impact of the risk of virus transmission to what is widely regarded as the new normal. The clinical adoption of telemedicine has been much slower (usually only used for special-use opportunities), however with this COVID-19 pandemic, there has been a surge in all digital communications.
Healthcare applications, especially telemedicine, has finally rapidly expanded, mainly because it enables physicians to remotely evaluate their patients. This can be advantageous for several reasons:
Telemedicine can assist to more efficient and reasonable distribution of constrained healthcare assets, by delivering support with innovative service design that already exists, to distant areas where there is a shortage of physicians and other healthcare professionals, by reducing travel transport challenges and the associated carbon footprint. Furthermore, in acute cases patients could receive immediate specialist input even if one is not available locally and access to care for both chronic and acute disease patients could be reduced while maximizing the quality of the telemedicine consultation.
During the COVID-19 pandemic, telemedicine is no more focused on only targeting remote regions, but it is rapidly becoming a new standard of care adopted by multiple centers across the world, as it enables triaging prior to patients arrival into hospital to avoid unnecessary visits and exposure risks.
1, 68Finally, the collection, storage and transmission of data offer the potential of combining telemedicine with AI and many other innovative technologies. When used prospectively with longitudinal data, vast swathes of new knowledge such as disease progression and real world, real-time incidence calculation could be harnessed. Moreover, this could grow into a consistent source of longitudinal data which would be valuable in the development of disease progression forecasting capabilities by training and incorporating AI.
2. Other Critical Supporting Infrastructures
Even as the Internet has been exponentially growing, and the communication systems (cabled and wireless) have likewise logarithmically increased, there are other parallel information-based technologies that have rapidly grown as well. In most cases, these technologies have developed in their own silo, usually due to inadequate communication systems to unite them. The emerging 5G wireless networks are finally providing the bandwidth, speed, and low-latency to act as a force to begin integrating these parallel technologies into an information ecosystem. What enables this huge increase is the change of the networking from connections by physical wires (cables), to wirelessly distributing the network using software (software designed networks SDN) and network slicing: an analogy of instead of laying another wire or cable, the software instead slices the wireless network into different frequencies when a new connection is needed. This allows the integration of other technologies, and most importantly the IoT which also supports robotics and sensor technology, BD acquisition, data repositories, AI, computational analytics, and supercomputing (Appendix 1).
The new telecommunications networks are not only connecting human to humans but also connecting smart devices (especially the 8 billion smart phones) of the IoT total of 14.2 billion devices now, with projections of 25 billion by 2025 and 60 billion by 2030. In addition, there is massive data acquisition continuously monitoring by microsensors from machines (devices, equipment, systems) or living systems including humans, most of which is machine to machine communication for maintenance and/or autonomous control and all linked together using Global Positioning System (GPS) for precise geolocation.
Careful attention must be paid to the interface between the HIT that provides the final connection of the communication system with a person, be it the current video technologies, or any of the forms of VR, or possible future interfaces such as wearable contact lens displays, or the ultimate brain-machine interface. After all, this information ecosystem is a system-of-systems, with each link in the chain dependent upon the success of all others, that decisively results in success.
4. Clinical Applications Using 5-G Wireless Networking
The current capacity of 5G telecommunications provide the perfect ecosystem to reassess care delivery and to adopt the synergistic and complementary digital technologies discussed above, incorporating AI utilization, and facilitated by 5G networks, IoT and BD and computational analysis. Below are some clinical applications of using 5G:
The following examples illustrate the large breadth of healthcare clinical services that can now be provided because of the emerging 5G networks.
Pulmonology
Up to now, there is conflicting evidence that telemedicine solutions help address chronic respiratory diseases.22
However, a recent paper (see ), profiting from the capacity to parallel several IoT applications due to the coexistence of multiple streams by 5G connectivity, presented a home telemonitoring system designed for chronic respiratory patients.
All data were streamed to an iPad which was connected via Wi-Fi to a 5G router and thereafter to the 5G infrastructure. The authors could access the data by means of a dedicated dashboard. The whole system was tested on 18 healthy volunteers during nonsupervised recordings lasting at least 48hours. Due to the 5G bandwidth, the results showed that the system provided more complete and clinically relevant and real-time information than other previously studied telemedicine systems.22
Medical Imaging and 5G
As a massive number of images accumulates and manual segmentation requires a lot of time, it becomes a big challenge for analyzing and diagnosing and furthermore, it may not meet the demand of analyzing big images data.23 This problem is attacked by using automatic methods for sectioning medical images (SMI) to obtain any viewing angle via multiplanar reconstruction (MPR) by using a plethora of various technologies, for example, region-based methods, clustering methods, threshold algorithms, machine learning, and deep learning.24
However, since each MPRs interaction requires the reconstruction of the raw data, thus hundreds of megabytes of SMI data must be transferred, resulting in a higher requirement for network transmission via Internet without a bottleneck creation as well as a higher security risk of data leakage.25 This is an example of the advantages and opportunity for 5G communication with Software Designed Networks (SDN) and network slicing to more flexibly, efficiently and cost effectively provide enhance Intranet and Internet capability and security.
Of course, this is not the case for less demanding imaging such as echocardiography or dermatology images transfer, where effective transmission of high-quality images can be accomplished either through low-cost transmission systems or with images/video from publicly available apps.26,27 The same applies to otolaryngologic exams, especially regarding remote of video-otoscopy images, as a recent review suggests that they can deliver adequate information suitable for diagnosis in most cases and results in high levels of user satisfaction.28
Diagnostic pathology is mainly depending upon image quality. The conventional cytological glass slide examination is time consuming as only one person can view it at a time. Beyond the use of the static images in telepathology, dynamic telepathology has recently been introduced, where the transmission of microscopic slide images to the recipient is done in real time via live telecommunication. Furthermore, through the implementation of remote robotic control of the microscope, the consulting pathologist can also control the magnification, a feature extremely useful for interoperative pathological analysis.29 The introduction of advanced, micro-miniaturized imagers, such as optical coherence tomography (OCT) and near infrared spectroscopy, are being introduced through gastrointestinal endoscopes, providing immediate ultrahigh-resolution images of intra-cellular structural pathology for the endoscopist,30 which can be streamed live to the consulting pathologist and/or archived for future reference.
Remote Ultrasonography
Much interest has been shown in robotic-assisted teleultrasound and expert remote consultation. During this procedure, the operator manipulates a simulated robotic hand to remotely control the robotic arm at the patient end. An ultrasound probe is fixed on the robotic arm to scan the patient. Up to 2GB of ultrasonic image data from a lung ultrasound scan lasting a few minutes is produced and transmitted at high speed with low latency. The robotic arm is movable and easy to use, allowing clinicians to collect lung images directly and monitor patients remotely.
From a technical point of view, the network download rate is 930 Mbps and the upload rate of 132 Mbps, maintaining a stable level with latency being at 2330ms and the network jitter at 12ms, thus allowing a smooth scanning by the robotic arm and an undetected time delay. No package loss was detected during all the procedures and thus the images quality transmitted to the attending physician had no visual reduction compared with those obtained by traditional on-site examination. Therefore, it is concluded that by breaking the temporal and spatial limitations due to the high bandwidth network, robotic-assisted teleultrasound succeeds in bridging the gaps between specialists and patients from remote cities.31 This real-time image acquisition of robotic ultrasound across long distances has the following advantages:
Examiners can be protected from cross infection by remotely monitoring patients without any personal contact thus diminishing the number of those who come into contact with the patients.
Experts by using this technology can remotely perform real-time ultrasound scan on patients in distant locations, thus alleviating the pressure of shortages of medical resources.
The robotic ultrasound can be performed anywhere, at the patients bedside or even in the patients home.
32
As can be seen from , there are three relevant articles using robotic teleultrasound lung scanning for suspected and/or declared COVID-19 patients, all originating from China:
The first article evaluated robot-assisted teleultrasound and expert remote consultation for early cardiopulmonary evaluation by performing lung ultrasound, brief echocardiography, and blood volume assessment in four patients hospitalized in isolation wards and the examination results were immediately delivered to the attending physicians. Furthermore, the authors report the use of this robot-assisted teleultrasound examination as a routine for evaluating acute abdominal diseases such as cholecystitis, appendicitis, pancreatitis, and urolithiasis. In addition, teleultrasound has been applied in focused assessment with sonograph for trauma (FAST) and extended FAST, musculoskeletal injuries, thyroid gland diseases, and subcutaneous soft tissue lesions.31
The second article used a robotic ultrasound system, integrating remote robotic control, audio-visual communication and ultrasound examination, and assessed its feasibility in 23 COVID-19 cases. Furthermore, they established a standard examination and evaluation protocol as follows: A cardiopulmonary assessment completed successfully for all patients lasting on average 10 to 20min. An ultrasound image contained information regarding distribution characteristics, morphology of the lungs and surrounding tissue lesions, left ventricular ejection fraction, right/left ventricular end diastolic area, pericardial and/or pleural effusion, and lung ultrasound score. Although they had excellent results in COVID-19 detection, they admit that the 5G robotic-assisted remote ultrasound system is still in its infancy, has several limitations (i.e. restrictions of the examination position of critically ill patients, limited operating angle of the robotic arm, use of only one ultrasound probe) and requires further improvements as well as multicenter trials to establish its feasibility as a valuable tool for remote lung pathology detection.33
The third article of two cases discusses the advantages of using US versus chest CT for detection of lung abnormalities due to COVID-19, stating that limitations of CT are: a) difficult to perform on patients in critical condition who cannot be moved. b) CT is not available everywhere, and c) the enclosed environment of CT may contribute to the spread of the coronavirus. On the other hand, ultrasound has the advantages of repeatability, absence of radiation, and ease of use. Compared with ordinary ultrasound, 5G remote robotic ultrasound has the added advantages of protecting operators, alleviating the pressure of medical equipment shortages, and considerable portability. The authors conclude that 5G remote robotic ultrasound may become a suitable choice for diagnosis and monitoring patients with COVID-19 infection.32
Ophthalmology
An excellent review summarizes the digital technologies applied across different countries which are expected to increase the clinical workflow of ophthalmologists.5 It is exactly because the data-rich image requirements needed in Ophthalmology that 5G, IoT and AI are introduced for OCT and fundus cameras and algorithms which are changing ophthalmological service delivery. These technologies are expected to enhance the quality and continuity of eye care to all patients.
Recently, a 5G connected smartphone attached to a portable slit lamp provided a live streaming in real time of high enough quality to be used clinically, thus opening up even more potential for telemedicine and teleophthalmology in the future.34
The implementation of these technologies remains challenging, including the validation, patient acceptance, and education and the training of ophthalmologists on these technologies. It is imperative that they must collaborate with technology experts and data scientists to achieve universal quality and sustainable ophthalmic services and continue to adapt to the changing models of healthcare delivery.5
Interventional Cardiology
Robotic telestenting, in which percutaneous coronary intervention (PCI) is performed on a remotely located patient, availability of 5G could improve patient access to PCI, but has not been attempted over long distances likely required to reach many underserved regions.
In a recent study cited in , telestenting performance was compared in regional (206 miles) and transcontinental (3,085 miles) distances from the interventional cardiologist. Ex vivo models of telestenting were used, and robotic PCI on endovascular simulators was attempted over both wired and 5G wireless networks and audio and video communications between the cardiologist and the simulation laboratory personnel were established over the network. A total of 20 consecutive target lesions in the regional model and of 16 consecutive target lesions in the transcontinental model were successfully performed. Outcome measures included procedural success, procedural time, and perceived latency. Procedural success was achieved in all lesions in both models. Latency was imperceptible in all cases in both models and the greater distance of the transcontinental model had not significantly different procedural times compared to the regional model for cases performed over wired or 5G-wireless networks.35 This is the first study which demonstrates that remote robotic manipulation of coronary devices is now possible using wireless network connectivity.
Emergency Medicine
The emergency department (ED) is a good example for the widespread introduction of virtual triage via telemedicine, rather than coming directly to the ED in person. The patients benefit as they are not obliged to attend in person and can be treated with remotely delivered prescriptions. If they do need to attend, an appointment time can be scheduled more efficiently, being seen directly by the specialists rather than spending long hours in the ED waiting room. Additionally, with the maturation of chatbots, much of the patients counselling can be performed flawlessly through video consultation. Additionally, the healthcare providers benefit from the absence of physical attendance, the costs associated with additional time and space utilization, as well as the use of personal protective equipment. The healthcare personnel who can work from home can contribute to the efficient use of human resources at a time where sustainability must also be considered. Reduced in person ED visits also decrease the general workforce risk of COVID- 19, avoiding the highly undesirable scenario of transmission between clinicians and patients.36 The safety and efficiency of remote triaging and automated counselling need to be evaluated, and until then, clinicians need to oversee each consultation as is standard process prior to the pandemic.
Obstetrics
So far, in an attempt to make accurate diagnoses in emergencies, smartphones are used to take videos transmitted in real time to consultants located at a central hospital who then can assess the situation.37 One such emergency is to estimate in real time the status of a fetus in utero through a cardiotocogram (CTG). However, it is used in medical care clinics only, and there are few reports attempting to send CTG data via a mobile network from home or from an ambulance to a medical institution. Several problems could occur and only one successful case has been published so far.38 With the deployment of 5G this solution could be implemented as described in a recent publication, where the authors simulated the feasibility to concomitantly transmit not only CTG but also real time fetus US videos as well with excellent results. Thus, except CTG, the images during ultrasound examinations were high-quality videos on patient actors, which were transmitted without problems.38 Thus, home monitoring of a fetus with the 5G system is a particularly useful application, which could create a new future for obstetric care.
Surgery
While the practice of a surgeon is very much like the practice of general medical practitioner, the distinguishing feature is the amount of time committed to performing surgical procedures upon their patients. Surgeons do have the same clinical, educational, research and administrative requirements as all physicians, including the basics of history, physical, lab/imaging studies, outpatient and in-hospital care, discharge and follow-up. Likewise, in response to the COVID-19 pandemic, this includes the increased use of teleconsultation, teleconferences, etc., which is anticipated to be continued upon resolution of the pandemic. However, like all healthcare specialties, there are additional unique requirements and opportunities, which is the focus of the following surgical areas:
Pre-operative preparation
Intraoperative procedure, and
Postoperative follow-up (both in hospital and outpatient care).
1. Pre-operative Preparation
The surgeon meets the patient in the pre-anesthesia area and needs access to all the medical information from the medical record for review which includes both medical data and medical images. If it is a complex procedure, many surgeons will not only have review of a full 3-D reconstruction of imaging studies (computed tomography [CT], magnetic resonance imaging [MRI], etc.), but may have also actually previously rehearsed the procedure using simulation, all of which requires real-time access to massive amounts of imaging data.
2. Intraoperative Procedure
More and more operations are being performed by minimally invasive surgery (MIS). Often, the video image is being captured, with the potential for sharing real-time with other surgeons or archiving. When used for educational purposes, high - bandwidth is needed for the transmission of the video image, along with audio for the surgeon to communicate with the learners in the audience. The archived video of the procedure can be used for many educational and administrative or legal purposes, including credentialling, privileging, or remediation. In addition, during surgery, the surgeon often will need to take a biopsy which is sent to a pathologist to be examined and reported back to the surgeon waiting for the results to complete the operation. New instruments now are able to capture the image of the pathology in real time and transmit the image directly to the pathologist for diagnosis, saving significant operative time. Telepathology can be in the same hospital, or literally anywhere around the world for consultation in difficult diagnostic cases. Another technology, data fusion, permits overlaying the live video image with additional images (CT, MRI, fluorescence markers, etc.) to guide surgeons with X-ray vision to see structures and pathology within organs or lymph nodes (for cancer).
3. Postoperative Care (Including Outpatients)
The immediate postoperative care of a surgical patient has previously been done within an in-hospital stay, however the newer MIS procedures have allowed many patients with simple, uncomplicated surgical procedures to go home the same day. Teleconsultation to the patients home, especially during the COVID-19 pandemic, has exponentially increased. Not only is there the opportunity to speak to the patient by using a cell phone, but it is now possible to actually see the patient and use the phone (or any one of the many new in-home medical devices to examine the site of the surgery, saving patients the need to come to the hospital for follow up. This capability for a visual examination is also in very high demand for many chronic nonsurgical diseases, especially for wound care and dressing changes.
Trauma and accident injury is a special needs surgical application because minutes to surgical care can be critical. Innovation in instruments, devices, procedures, and training, including the Advanced Trauma and Life Support (ATLS), has dramatically increased the lives saved. The new capabilities of communicating with an ATLS trained responder, especially in a telemedicine-enabled ambulance, can bring a sophisticated trauma surgeons consultation directly to a first responder anywhere. Because of the militarys need for (and research in) battlefield trauma care, it is anticipated that a significant increase in remote, telemedical care (including the possibility of remote telesurgical care) will be enabled by the scope of 5G communications.
Clinical Telesurgery
Telesurgery (or remote surgery) aims to break the obstacle of geographical boundaries in providing high quality healthcare in the most complex medical interventions and surgeries. High-qualified medical expertise will be transferred from the major hospitals to the decentralized ones with the use of remote-surgery, remote diagnostics and telemedicine resulting in significant cost reduction, and improved efficiency in health care services. Telesurgery, where parts of the procedure are controlled by a surgeon from a central site to a remote location, is the most demanding application among the remote healthcare services and thus by successfully validating this application, the validation of technology for the entire range of less demanding remote healthcare applications can be implied.39
The domain of applications of remote surgery, apart from decentralizing health care, are remote surgical operations under extreme conditions, such as at the battlefield and remote operations in extreme environments like in space missions. Telesurgery entails the use of a master-slave robotic surgical system. Currently, the only Robot-assisted Minimally Invasive Surgery (RAMIS) system with FDA approval is the da Vinci surgical system, which has offered to surgeons a greater visualization, enhanced dexterity, greater precision and greater comfort; to the patients it has offered shorter hospitalization times, reduced pain and discomfort and faster recovery time.
As can be seen from there are very few clinical reports using 5G for telesurgery. For example Remote RAMIS (telesurgery) has already had investigational testing in various scenarios and conditions.40,41 The first true telesurgery on a patient was performed in 2001 between New York, USA and Strasbourg, France (6200 km apart); the so-called Lindbergh Operation.42 The authors used a dedicated trans-Atlantic fiber-optic cable. The average round-trip delay was 155ms including delays in image transmission, which made delay of movements executed by the surgeon in NY, apparent but easily managed within the 155ms. Telesurgery has since been performed by other researchers. Anvari and colleagues43 have reported the largest patient series with more than 30 remote operations between the central site located in Hamilton, Canada and the remote site in North Bay, Canada (400Km apart), over a virtual private network (VPN) on a nondedicated fiber-optic line. Reported average latency was 140ms which was noticeable by the surgeon, who automatically compensated for the delay. It has been suggested that the ideal latency time for telesurgery should be less than 100ms and that problems such as inaccurate manipulation could appear if the latency time is longer than 300ms.44 All aforementioned research outcomes do not include haptic feedback, which severely increases latency. It has yet to be tested whether future telesurgery systems will be able to integrate haptic feedback that is accurate and precise enough to increase the surgeons performance without increasing latency.
In order to implement remote surgery, we should address the critical technical challenges of robotic telesurgery, which are the minimization of latency between master-slave and the maximization of reliability, availability and security of the communication channel. The desired specifications are:
Latency (end-to-end round trips) of 100ms depending on the application.
Ultrareliable communications (seven nines).
The term ultrareliable can be quantified in terms of fixed-line carrier-grade reliability of seven nines i.e., an outage probability of 107, which translates to microseconds of outage per day. These specifications cannot be provided today by existing 3G and 4G networks.
The hypothesis is that 5G infrastructure offers the desired reliability and latency and therefore is an enabler for safety-critical applications such that remote surgery, from a central major surgical hospital medical center can be matched to a specific patients medical needs in a remote hospital location. In the more distant future, when haptic technologies develop to a safe level of precision and accuracy, these technologies can be applied to RAMIS telesurgery systems. It should be noted that the same infrastructure of haptics for telesurgery could be applied to other remote healthcare applications such as telediagnostic tools, which could be available anywhere, anytime, allowing remote physical examination which could include palpation.45
As with all newly implemented emerging technologies like telesurgery, facilitation by the 5G network is a game changer. Highly delicate procedures like spinal surgery could benefit from high capacity, low latency. This also applies to other surgeries in other specialties like cardiac surgery, urology, and colorectal surgery. In short, the entire domain of surgical procedures could be enhanced with 5G enabled telesurgery.
Before 5G, only a few telesurgeries were reported which were carried out through a 4G network while mostly internet and satellite networks were previously used for telesurgery.46 Thus, Wirz et al.. performed robotic telesurgery to complete a pituitary tumor resection on a simulated model over the Internet with a bandwidth of 1Gb/s in 2015.47 Regarding surgical applications our review revealed two preclinical studies: One article reporting 5G mediated nephrectomies in 4 swine, estimating the latency time due to long (300Km) distance,48 and another one operating in 5 pigs in a shorter distance (16Km) 40 Rayman et al. performed robotic telesurgery to perform a left internal mammary artery dissection in pigs through a satellite network with a maximum bandwidth of 10Mb/s.49
Regarding remote telesurgeries, in USA, a surgeon from Texas, 1200 miles away from a Florida Hospital, remotely manipulated the da Vinci robot, performing operations on simulated patients through the Internet. In China, Hainan Hospital of Chinese PLA General Hospital and Beijing Jishuitan Hospital performed remote positioning for brain pacemaker implantation surgery and screw fixation surgery, respectively, through a 5G network. However, these surgeries do not require high demands on network latency and bandwidth of the 5G network as compared to the continuous manipulation and 3D video transmission in laparoscopic surgery.48,50
While the future for telesurgery looks bright, there are a number of challenges that need to be addressed. The following are suggestions for research studies:
Both the surgeon console and the patient side cart need to be more compact or portable. Ultimately, the surgeon console could be as portable as a laptop computer and the patient side cart should be compact so that it can be placed in an ambulance or a mobile ward (En-route damage-control surgery).
Surgical robots need to be combined with AI, capable to alert of dangerous actions during the operation (error prediction and hazard avoidance).
Protocols and responsibilities need to be clearly defined to define whether causation of errors is from device (robotic and/or telecommunication system) or surgeon control.
Communication corporations need to take measures to assign and guarantee enough bandwidth and high priority for telesurgery.
With network security is still one of the major challenges to telesurgery, a security guard system for the 5G network has to be designed and implemented (anti-hacking).
Telerobotic Spinal Surgery
It is well known that robot-assisted spinal surgery has been a popular and reliable surgical procedure. Furthermore, a recent meta-analysis showed that the accuracy of robot-assisted pedicle screw placement was significantly higher than the freehand method.51
A recent study () in which 6 hospitals participated from 6 different cities in China, 5G telerobotic spinal surgeries for 12 patients were performed and a total of 62 pedicle screws were successfully implanted using the 5G telerobotic surgery system.52 The operation time was 142.546.7minutes, and the mean guide wire insertion time was 41.39.8minutes without any intraoperative adverse events. They concluded that telerobotic spinal surgery based on the 5G network is accurate, safe, and reliable. The application of the 5G network in the clinical area has great potential and value in the future.
The authors also explored the new pattern of one-to-many remote surgery. Under this mode of remote surgery, one expert surgeon can simultaneously provide surgical care to more than one remotely located hospitals, something which previously was significantly restricted by the limit of network bandwidth. A one-to-three telerobotic surgery was successfully performed during this study, and it is believed that even more multicenter remote surgery is simultaneously possible, due to the vast potential of the 5G network.52
Future Directions
A reflection on the enormous number of advanced technologies rapidly occurring in this new Information Age emboldens the authors to make certain extrapolations of known advancements in science to suggest forward-looking statements about likely technology outcomes for the future. However, It is apparent that some of the emerging technologies, such as, 5G communications, AI, telemedicine (and telesurgery), automatic image interpretations, genetics, proteomics58,59 and others are radically (and rapidly) changing the practice of medicine. Two areas need to be addressed: The core technologies in 5G communication, that are supporting most every industry and the healthcare specific technologies for medical needs.
The assumption is that the 5G and subsequent generations of wireless communication technologies will provide service now and in the future with exponentially increasing bandwidth (for data/information flow), decreasing latency (for real-time, near-real-time or just-in-time requirements) and with reliability/availability (the seven nines 99.99999% reliability), usability (simple human/machine interface), accuracy (received/delivered to the correct person/location), and especially security/privacy. The second assumption is that while the transmitting and receiving of information must obey physical laws, the interfaces (devices) for humans must obey both physical laws and biologic limitations [Note: machine-to-machine interfaces only obey physical laws].
Finally, attention must also be paid to the type of supporting technology requirements, such as AI to enhance human intellectual performance in solving problems, supercomputers and BD repositories, sensors/actuators and MEMS on the IoT for data acquisition, etc., which are driving the need for better communication networks.
Surgery is in its fourth generation (Open surgery, endoluminal surgery, laparoscopic surgery, and now robotic surgery) with the emerging fifth generation of surgery being directed energy. The trend is for less invasive procedures (endoluminal) through natural body openings (mouth, nose, rectum, ears, etc.) to perform surgical procedures. This has been followed by and today the newest generation is robotic assisted minimally invasive surgery (RAMIS). Postoperative follow-up visits are being performed with teleconsultation. Until now, only a few remote surgeries (telesurgeries) have been performed because of the connecting cable between the surgeon console and robot arms. It is anticipated that the wireless 5G networks, with huge bandwidth and low latency, will lead to more implementation of telesurgery.